In This Article
We are one of a handful of clinics that is able to accept insurance for ketamine therapy. Obtaining insurance coverage for ketamine treatment can be complicated, so our team is committed to making the process simple.
If your plan is in-network, Ketamine Wellness Centers will work directly with your insurance company to determine your eligibility for coverage. If your insurance plan is out-of-network, there are still steps we can take to help you pursue reimbursement.
Understanding Insurance Terms
The exact cost of ketamine therapy depends on specific aspects of your insurance plan, such as whether you’re in-network, if you need prior authorization, and your required copay. After our team processes your insurance, you will receive a detailed email from KWC breaking down your estimated cost based on these factors.
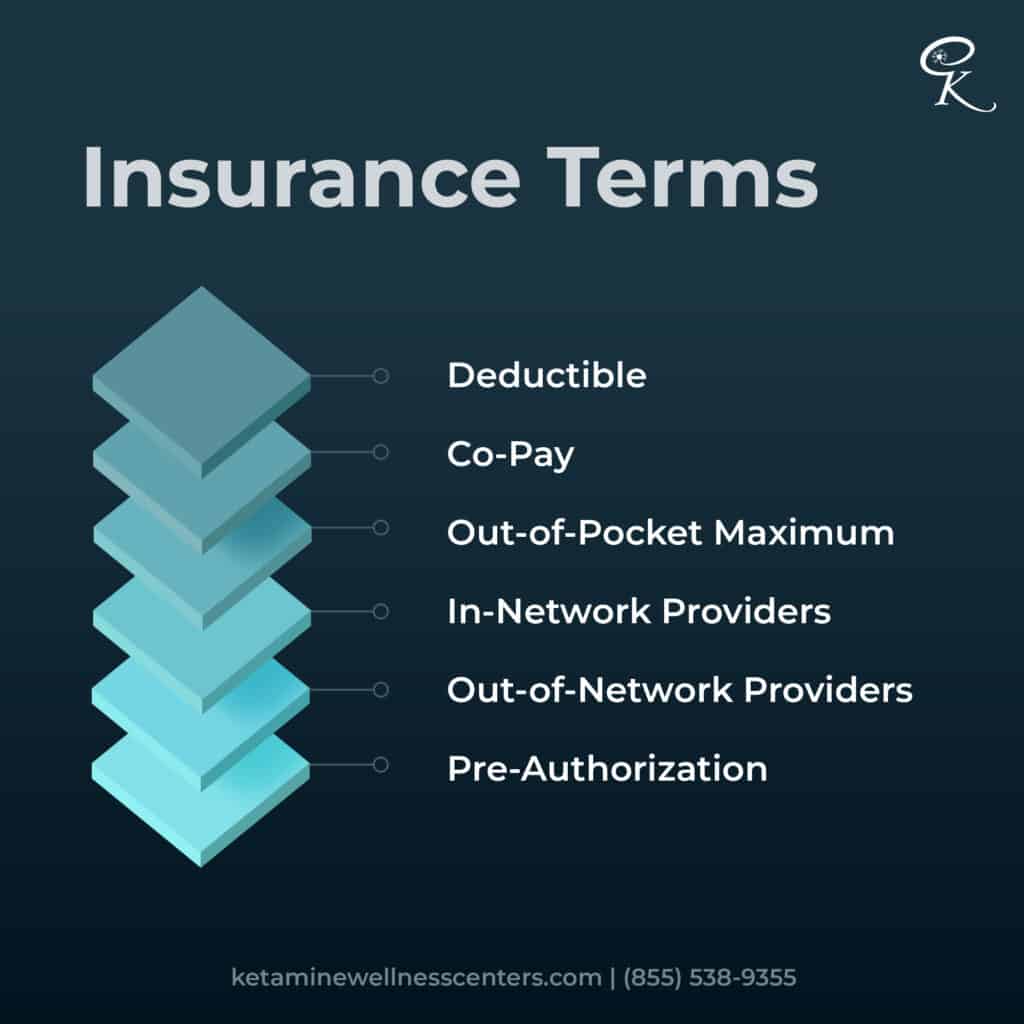
In-Network vs. Out-of-Network
Certain health insurance companies will cover a portion of the cost of ketamine treatments. A company that is “in-network” with Ketamine Wellness Centers offers treatment coverage to eligible patients.
Prior Authorization
Sometimes, insurance will only cover a treatment or procedure if the patient receives prior authorization. This means that a healthcare provider submits a request for insurance coverage before providing treatment.
Superbill
Your superbill is an itemized list that breaks down the charges on your bill. Even if your insurance does not cover ketamine therapy, you may be eligible for reimbursement for your office visit, medical monitoring, and any additional medication you receive. Submitting a superbill to your insurance company can lead to additional treatment discounts.
Out-of-Pocket Maximum
Each year, your insurance company determines the maximum amount of money you will be required to pay for covered medical services. For example, if your out-of-pocket maximum is $8,000, your health insurance company will pay for all covered healthcare services for the rest of the year after you’ve spent $8,000 on covered healthcare.
Copay
Your copayment (or “copay”) is the fixed amount your insurance charges for covered medical services like doctor visits, prescriptions, and lab tests. If your ketamine treatment is covered by insurance, your copay for specialty visits will determine what you owe.
Treatment Options at Ketamine Wellness Centers
Our clinics offer both infusions and nasal spray as options for ketamine therapy. Since insurance coverage is determined on a case-by-case basis, you may find that one of these options is covered while the other is not. Your eligibility for coverage depends on factors like your insurance plan, diagnosis, medical history, and the form of treatment you pursue.
Ketamine Infusions
IV (intravenous) infusions are the most common form of ketamine therapy. While many ketamine clinics cannot accept insurance, KWC has has partnered with several insurance companies to offer discounted rates for eligible patients.
KWC offers ketamine infusions for both mental health and chronic pain conditions. Typically, insurance companies will offer different levels of coverage for different conditions. For chronic pain patients, a medical pain diagnosis such as fibromyalgia, migraines, or Complex Regional Pain Syndrome is usually required to obtain coverage. For mental wellness patients, the patient may need to demonstrate that other treatments (such as medication and psychotherapy) have not been effective.
SpravatoⓇ Nasal Spray
Spravato (esketamine) is a form of ketamine specifically developed for treatment-resistant depression. Because Spravato is FDA-approved for this purpose, it is much more likely to be covered than infusions for depression.
To be eligible for Spravato treatment, the patient must meet the criteria for a diagnosis of treatment-resistant depression (TRD). If you’ve been prescribed two or more antidepressants without finding sufficient relief, talk to your healthcare provider to see if you may be suffering from TRD.
Get Help from our Insurance Specialists
Our team understands that even before insurance is involved, seeking help can feel overwhelming. To make your road to treatment easier, our insurance specialists can navigate the majority of the process for you. We will:
Obtain Prior Authorization
Obtaining prior authorization is an essential step in qualifying your treatment for reimbursement. While it does not guarantee coverage, your insurance company may require a prior authorization request before you are considered eligible. If your insurance plan is in network with KWC, our team will take care of this on your behalf.
Work With Your Medical Provider
Before you can begin treatment, your care team will need to obtain information about your medical history. With your permission, we can contact your medical provider to gather information (like medical records and referrals)–meaning you won’t need to obtain these records yourself.
Provide a Superbill
The cost of your treatment is broken down into specific charges: the office visit, monitoring equipment, and medication itself are all separate items on the bill. This means that even if ketamine is not covered by your insurance, other aspects of your treatment may be reimbursable.
Even if your plan is not in-network, you may receive some reimbursement after submitting a superbill. Some of our patients have been automatically reimbursed for a percentage of their treatment cost just by submitting the superbill to their insurance company.
After we’ve contacted your insurance provider, determinations about your coverage may be made in as little as 48 hours. We are available throughout this process to answer your questions and help you decide the best course of action for your care.
Your Next Steps
If you are suffering and have been considering ketamine infusions, our team is here to help you get started. To ask questions, receive more information, or move forward with treatment, you can contact us at:
Email: insurance@ketaminewellnesscenters.com
Phone: 855 KET-WELL / (855) 538-9355
Even after being told that insurance was unlikely to cover anything, many of our patients have succeeded in finding treatment reimbursement. At KWC, we believe that cost shouldn’t be a barrier to wellness–and we want to help.
Further reading: Cost of Ketamine Infusion Therapy